Background: Guidelines recommend placement of inferior vena cava (IVC) filters in patients with acute thrombotic episodes and a concurrent contraindication to anticoagulation, however filter placement during or immediately postpartum presents significant technical challenges. The use and complications of IVC filters in the peripartum period is poorly documented in current literature.
Objective(s): To evaluate the use of and outcomes related to IVC filters in an obstetric population at a large tertiary care center.
Study Design: Retrospective review of all patients at a tertiary academic medical center from 2001-2016 who either conceived with an IVC filter in place or underwent IVC filter placement during the antepartum or postpartum interval. Manual abstraction of each chart was performed, with data stored in a RedCap database.
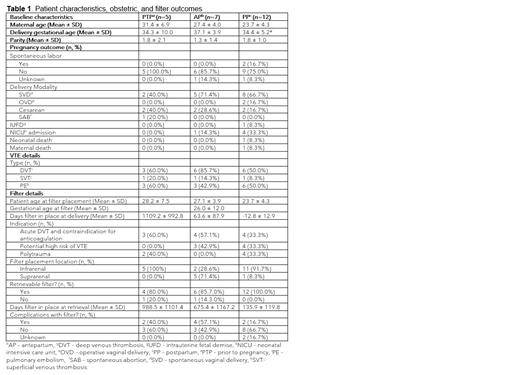
Results: A total of 24 patients were included in the final analysis: 5 with IVC filter placement prior to pregnancy, 7 with antepartum placement, and 12 with postpartum placement. One patient had multiple pregnancies during our study timeframe and was therefore included twice. The cohort of postpartum placement were the youngest mean age (23.7 years), had a higher number of IVC filters placed for polytrauma (n=4), and had the shortest time to removal (135.9 days). The vast majority (91.3%) of IVC filters placed during pregnancy were retrievable filters in the suprarenal position, while most deployed in an infrarenal position (83.3%) when placed prior to conception. Complications encountered included multiple attempts to remove IVC filter, severe angulation, embedded struts, fracture, and one case of cardiac tamponade during filter placement requiring emergent sternotomy and evacuation. Of the filters requiring multiple attempts for removal, in 1 patient (4%) it was unable to be removed despite multiple attempts and the filter was ultimately left in situ. Complications were more common when placement was performed prior to pregnancy or antepartum (40% and 57.1% respectively) versus postpartum (16.7%). From an obstetrical perspective, 1 patient (4%) required early preterm delivery due to preeclampsia; 1 maternal death occurred in a postpartum patient who experienced a massive pulmonary embolism and subsequently died despite emergent thrombectomy and IVC filter placement, and 1 neonatal death occurred due to congenital heart disease following periviable preterm delivery.
Conclusion(s): In our study across 16 years at a large academic medical center we identified 23 patients who had an IVC filter placed prior to pregnancy or placed during the antepartum or postpartum periods. Data from our experience suggested a higher incidence of complications with preconceptual and antepartum placement, although the majority of these did not impact clinical outcomes. While not frequently needed, IVC filters remain an option for clinicians treating pregnant and postpartum patients but should be considered a last resource as they can lead to various complications.
Disclosures
No relevant conflicts of interest to declare.